Donation has long been considered a noble cause. But there have always been opponents. This article is not for them. Blood is always needed in medicine. There is a catastrophic shortage of free enthusiasts, so medical institutions offer money for donating blood. In this article we will talk about blood donation, how much they pay for it in Russia and other countries.
Prices for donor blood vary greatly (from 150 to 4000 rubles in Russia) and are determined by several factors. The first one is demand. If you are planning to donate blood for money, it is best to first talk with the reception center employees to find out which medical institution needs the blood most. That's where you should head. In addition, a very important factor is the health status of the donor and the absence of bad habits. A person who has previously had hepatitis of any type or has blood-transmitted diseases can no longer be a donor. If bad habits missing, you lead healthy image life, the body is healthy, then the price of blood is naturally higher.
Another decisive factor is the blood type and Rh factor. The rarer the blood type, the more they pay for it. The fourth group is the rarest, since its owners make up only 5% of the total population of the planet. Even fewer people with the fourth group are Rh negative.
Cash payments for blood donation, amount and conditions
If we talk about blood donation, how much they pay, then the payment depends on what the donor donates: simply the amount of blood or its elements. For example, in December 2011, the following monetary payments were established: for 100 ml of whole blood - 650 rubles, for 100 ml of hardware plasmapheresis plasma - 400 rubles, for the procedure of double hardware erythrocytophyresis - 6000 rubles, for the procedure of hardware thrombocytopheresis - 4500 rubles. With all this, compensation for food in the amount of 1000 rubles is provided. Although, from other sources it follows that this compensation ranges from 400 to 650 rubles. If you have to donate 30 ml of blood for laboratory determination of your blood group, then this volume is not included in the amount of donated blood. Therefore, it is better to determine the blood type and Rh factor once and put the corresponding information in the passport and certify it with the seal of a medical institution.
When free blood donation, compensation for food on the day of blood donation is provided in the amount of 400-650, 1000 rubles (different sources vary). The more times a donor donates blood. The more he gets monetary compensation. For example, from the fifteenth to the twenty-fourth plasma donation, the donor is paid 500 rubles. for each change. Up to the fortieth time inclusive, they pay 1000 rubles. for one change, and after 40 times - 1500 rubles.
Labor legislation provides benefits for donors. On the day of blood donation, they may not go to work, but the rate remains the same. If the day of donation fell on a paid vacation, then the employee who donated blood can choose the day to rest after the end of the paid vacation. Of course, after providing them with the relevant certificates to the personnel department or accounting department at the place of work. People who have donated two or more units of blood in a year have priority to receive preferential vouchers at the enterprises where they work or study.
But people who decide to be donors should remember that no matter how much money it costs, they should not do it to the detriment of their health. When donating blood, it is important to follow the rules of nutrition, rest, and drinking regimen. Regular donors (blood donations occur three or more times a year) provide the blood transfusion center with certificates from doctors stating that there are no contraindications to donation.
By the way, it is worth noting that if you have, then, most likely, you will be prohibited from donating blood. So keep this in mind and take your time.
In the medical procedure of blood transfusion, at least two participants are involved: one of them, who provides his blood for transfusion, is called a donor among specialists, the other, to whom the transfusion is carried out, is called a recipient. To select a suitable donor for a recipient, several key factors must be taken into account.
Factors of blood compatibility between donor and recipient
One of the key conditions that determine the possibility of using the blood of a specific donor for a specific recipient is the compatibility of their blood groups. A blood group is a specific set of proteins in the blood of a particular person, and in nature there are only 4 variants of such combinations. In accordance with this, it is customary to distinguish 4 main blood groups, which are designated by serial numbers, or codes used in the AB0 system. Thus, the first blood group in this system is usually designated by code 0, the second by A, the third by B, and the fourth by AB.In addition to blood group, there is one more important condition, which determines the compatibility of the donor and recipient for the transfusion procedure. We are talking about the presence or absence in the human body of a special D-antigen, which is called the Rh factor. Accordingly, the concept of a positive Rh factor refers to the presence of this gene in the body, and a negative Rh factor refers to its absence.
Donor blood for a carrier of group IV
A person with blood group IV has the greatest chance of finding a suitable donor compared to other types of recipients. The fact is that it is the carriers of this group who have the widest compatibility with carriers of other groups; if they act as recipients, they are sometimes called universal recipients.However, it should be taken into account that the compatibility of a donor with a recipient having blood group IV will depend on the Rh factor of the latter. So, if he has a positive Rh factor, suitable donors for him will be those with all possible blood groups: I, II, III and IV, both with positive and negative Rh factor. A carrier of blood group IV who has a negative Rh factor will have a somewhat narrower circle of potential donors: in this capacity, those with all four blood groups, but only those with a negative Rh factor, will be suitable.
Group IV carrier as a donor
If the owner of blood group IV wants to act as a donor, then it should be borne in mind that in this case only a carrier of the same IV group can act as a recipient. Moreover, if the donor has a positive Rh factor, the recipient must also have a positive Rh factor. If a donor with group IV is the owner negative rhesus, his blood can be transfused to a carrier of the same group, both negative and negative Rh positive.Different blood groups have a number of distinctive components that can be negatively reflected when combining the two different groups. This phenomenon is explained by the presence on the surface and in the plasma of each individual group of an individual combination of agglutinins and agglutinogens, which are able to distinguish a foreign red blood cell from its own and prevent it functioning inside the body. The human immune system perceives cells with foreign agglutinogen as a threat. And for protective purposes, the body seeks to damage and remove them with the help of agglutinins contained in the plasma of its red blood cells.
Even before the beginning of the 20th century, it was believed that any blood could be combined, which was fundamentally wrong. And sometimes it even ended in death, since the transfused blood was not accepted by the body. The adhesion and destruction of red blood cells developed. But thanks to K. Landsteiner, who was able to detect and prove the presence of agglutinogens and agglutinins in erythrocytes, blood groups are now distinguished, and the blood transfusion scheme has become safe.
Blood groups
The system developed by Landsteiner is called ABO. It classifies four blood groups depending on agglutinogens, designated A and B, and agglutinins a, b in the composition.
Agglutinogens (antigen) are complex substances located on the erythrocyte membrane that are unchanged and inherited from their parents.
Agglutinin (antibodies) are immunoglobulins produced naturally in the plasma of red blood cells to protect the body from genes that are absent on the surface of the red blood cell. They are produced during the first year of life as a protective function of the immune system against the ingress of proteins with foreign antigens.
As can be seen from the table, each blood group differs in the set of antigens and agglutinins that are developed to the missing antigens for protection. 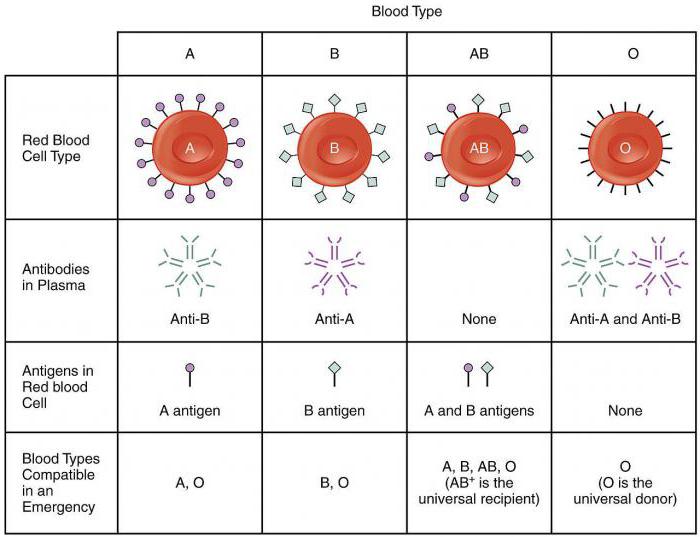 The plasma of red blood cells produces agglutinins of the opposite type from the antigens on the membrane. This opposition exists so that when red blood cells of a foreign blood type enter the body, they are quickly destroyed by antigens, without harming their own cells.
The plasma of red blood cells produces agglutinins of the opposite type from the antigens on the membrane. This opposition exists so that when red blood cells of a foreign blood type enter the body, they are quickly destroyed by antigens, without harming their own cells.
Blood Rh factor
In the scheme of blood transfusion of groups of acceptable combinations, it is also necessary to take into account the Rh factor of the blood. The Rh factor is a constant characteristic that does not change over the course of life and is a classification of blood according to the Rhesus (Rh) system. The Rh system is based on the identification of six antigens C, D, E, c, d, e on the surface of red blood cells, and was discovered in 1940 by K. Landsteiner and A. Weiner.
If antigen D is detected on the surface of red blood cells (found in 80% of people) or the simultaneous presence of antigens C and E, then the blood belongs to the positive Rh factor, designated Rh+. If no antigens of this group are detected, the Rh factor will be negative Rh-. 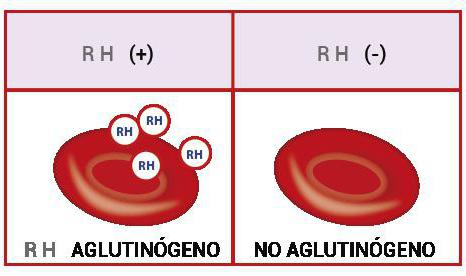
The importance of the Rh factor during transfusion
Blood that has the same Rhesus values is allowed for transfusion. So, for a recipient with a negative Rh factor, only donor blood with a negative indicator is suitable. The same is true with a positive one, however, in critical cases, infusion of blood with a negative Rh factor in small quantities, maximum 200 ml, is allowed. With such a transfusion, incompatibility does not occur, but when red blood cells with a positive value are infused into blood with a negative Rh factor, a protective reaction of the immune system to antigen D is observed. If foreign red blood cells are detected the immune system begins to produce agglutinins (d, c, e), which damage the infused red blood cells, which entails serious consequences for the recipient’s body. According to the Rhesus and ABO systems, a total of eight blood types are distinguished. 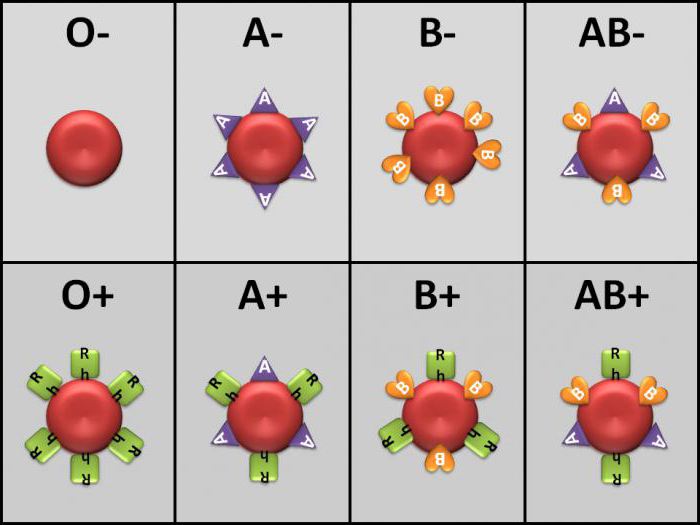
Blood compatibility
Hemotransfusion is a blood transfusion procedure that is used to restore blood balance and blood circulation. Donor blood must be compatible in both blood systems with the recipient's blood. For a long time it was believed that there is a universal donor and a universal recipient. At the moment, both of these concepts have already been practically extracted from the medical system. However, in critical situations, in the absence of time and donor blood of an identical group and Rh factor, it is sometimes still used in small volume transfusions, no more than 500 ml.
The universal donor includes blood of the first group and a negative Rh value of 0(I)Rh-, since it does not contain its own antigens. The fourth positive group AB(IV) Rh+ is considered a universal recipient, due to the presence of antigens A and B on the membrane of red blood cells. But, nevertheless, they try to carry out the transfusion procedure with identical groups. 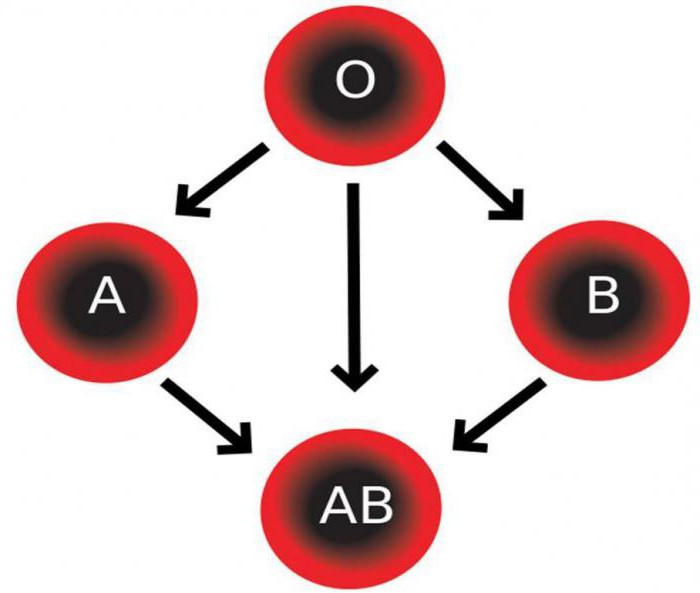
Blood group I: compatibility scheme
During transfusion, group I with a negative Rh value (0(I)Rh-) can be a donor for all blood groups with positive and negative Rh factor in case of emergency transfusion and, if a large volume is needed, act as a donor for group I with an identical Rh value.
For a recipient with the first blood group and positive Rh factor Donor blood can be the first positive or negative group 0(I)Rh-/+. In case of the first blood group with a negative Rh index, transfusion is performed only with an identical group 0(I)Rh-.
Second group compatibility
Second negative group A(II)Rh- can become a donor for the second and fourth with any Rh index. The second positive group A(II)Rh+ is used as a donor only for the second and fourth AB(IV)Rh+ with a positive Rh factor.
Recipient from the second positive group A(II)Rh+ can accept donor blood of the first 0(I)Rh-/+ and the second group A(II)Rh -/+ with any Rh index. If the recipient's blood is indicated by a negative Rh A(II)Rh value, the transfusion is performed with the same groups as for the second positive, only with an exclusively negative Rh factor value.
Third group compatibility
As a donor, third blood group with a positive Rh factor B(III) Rh+
used for transfusion to recipients of the third and fourth groups with a positive Rh index. The third negative group is compatible for donation with the third and fourth blood groups, regardless of the value of the Rh factor in the recipient.
Holders of the third positive group are transfused with donor blood of the first and third groups with negative or positive Rh. The third negative is characterized by compatibility with the third and fourth groups with a negative Rh factor.
Group 4 compatibility
Donor blood of the fourth group with a positive Rh factor is only suitable for transfusion to recipients with an identical group and Rh factor. The fourth negative group is also compatible for transfusion only with the fourth group with negative and positive Rhesus.
But a recipient with the fourth positive group AB(IV)Rh+ is universal and, with a positive Rh value, accepts absolutely all blood groups with any Rh values. At negative Rh factor During transfusion, donor red blood cells of all groups are used only with a negative Rh index. 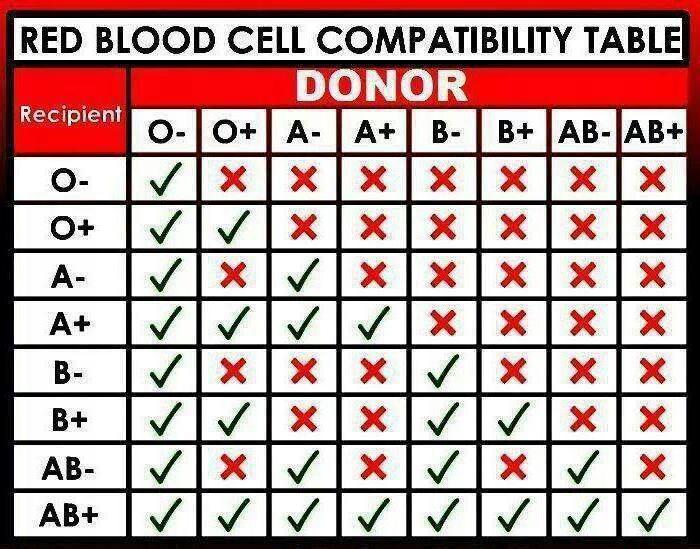
Risks of transfusion of incompatible groups
The main risk of blood transfusion is agglutination.
Agglutination is the process of gluing red blood cells, which leads to their destruction, and develops when blood with an agglutinogen enters the body, to which the recipient’s blood has produced agglutinin. This means that agglutination occurs when blood combines with the same antigens and agglutinins A and a, B and b. With this combination, antibodies (a or b) produced for the missing antigen (A or B) destroy donor red blood cells, resulting in their sedimentation and subsequent hemolysis (decay). 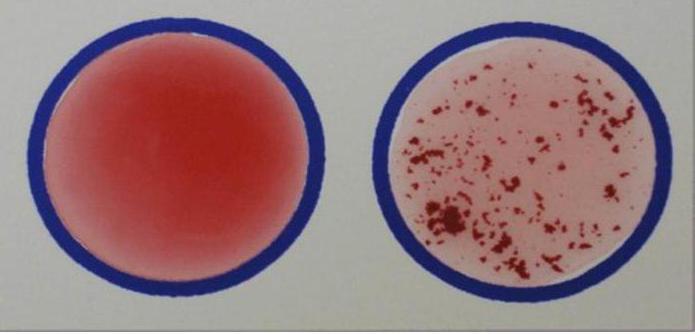 Blood is the main transporter of oxygen throughout all cells of the body, therefore, subsequent breakdown of red blood cells results in blood transfusion shock, which can cause severe consequences and even death. It is precisely on the basis of such risks that much attention is paid when blood transfusions to blood group schemes that are compatible with each other.
Blood is the main transporter of oxygen throughout all cells of the body, therefore, subsequent breakdown of red blood cells results in blood transfusion shock, which can cause severe consequences and even death. It is precisely on the basis of such risks that much attention is paid when blood transfusions to blood group schemes that are compatible with each other.
The ABO and Rhesus system is the main one for classification, but not the only one. On the surface of the red blood cell membrane there are many other antigens that are currently involved in the selection of compatible donor blood. But, more and more private clinics additionally determine the presence or absence of the rare Kell antigen, whose positive value makes donor red blood cells incompatible with any others.



