Today I went to get the test results for my blood group and Rh factor, I have 3, positive! This is good, because there will be no conflicts!!! (My husband has 4 positive)))
Inheritance of blood groups
Parents with the first blood group can only have a child with the first group.
Parents with the second have a child with the first or second.
Parents with the third have a child with the first or third.
Parents with the first and second have a child with the first or second.
Parents with the first and third have a child with the first or third.
Parents with the second and third have a child with any blood group.
Parents with the first and fourth have a child with the second and third.
Parents with the second and fourth have a child with the second, third and fourth
Parents with third and fourth- a child with the second, third and fourth.
Parents with the fourth have a child with the second, third and fourth.
If one of the parents has the first blood group, the child cannot have the fourth. And vice versa - if one of the parents has a fourth, the child cannot have a first.
Antigen B matures by the age of one year, so it is sometimes not detected at birth. As a result, a child with the third blood group may receive the first blood group at birth, while a child with the fourth may receive the second. By the age of one year, the antigen matures and the blood type “changes.”
Group incompatibility:
During pregnancy, not only Rh conflict (cm) can occur, but also blood group conflict. If the mother has the first blood group, and the child has any other, she can produce antibodies against it: antiA, antiB. It is necessary to check the presence of group antibodies in women with the first blood group, and in the presence of immune antibodies, warn pediatricians about the possible development of hemolytic disease of the newborn based on blood group.
Rh factor
Protein on the membrane of red blood cells. Present in 85% of Rh-positive people. The remaining 15% are Rh negative.
Inheritance: R - Rh factor gene. r - absence of Rh factor.
Parents are Rh positive (RR, Rr) - the child can be Rh positive (RR, Rr) or Rh negative (rr).
One parent is Rh positive (RR, Rr), the other is Rh negative (rr) - the child can be Rh positive (Rr) or Rh negative (rr).
The parents are Rh negative, the child can only be Rh negative.
The Rh factor, like the blood group, must be taken into account when receiving blood transfusions. When the Rh factor enters the blood of a Rh-negative person, anti-Rh antibodies are formed to it, which glue Rh-positive red blood cells into coin columns.
Rhesus conflict
It can occur during the pregnancy of an Rh-negative woman with a Rh-positive fetus (Rh factor from the father). When fetal red blood cells enter the mother's bloodstream, anti-Rh antibodies are formed against the Rh factor. Normally, the blood flow of the mother and fetus mixes only during childbirth, so a Rhesus conflict is theoretically possible in the second and subsequent pregnancies with an Rh-positive fetus. In practice, in modern conditions, there is often an increase in the permeability of placental vessels, various pathologies of pregnancy, leading to the entry of fetal red blood cells into the mother’s blood during the first pregnancy. Anti-Rh antibodies can also be formed not only during pregnancy, but also through contact with Rh-positive blood. Therefore, anti-Rh antibodies must be determined during any pregnancy in an Rh-negative woman starting from 8 weeks (the time of formation of the Rh factor in the fetus). To prevent their formation, carry out prevention of Rhesus conflict. All Rh-negative women who do not have antibodies to the Rh factor at 28 weeks of pregnancy are given anti-Rhesus immunoglobulin at a dose of 350 mcg. And another dose is given within 72 hours after birth. Immunoglobulin is also administered after any end of pregnancy of more than 8 weeks (miscarriage, abortion, anembryonia, frozen pregnancy, premature birth) and during the amniocentesis procedure. During pregnancy, it is possible to use only imported immunoglobulin preparations, in particular Bay-RoDee. After pregnancy, it is possible to use domestic immunoglobulin, which is better than nothing, but worse than an imported drug standardized in terms of the dose of antibodies.
Today I went to get the test results for my blood group and Rh factor, I have 3, positive! This is good, because there will be no conflicts!!! (My husband has 4 positive)))
Inheritance of blood groups
Parents with the first blood group can only have a child with the first group.
Parents with the second have a child with the first or second.
Parents with the third have a child with the first or third.
Parents with the first and second have a child with the first or second.
Parents with the first and third have a child with the first or third.
Parents with the second and third have a child with any blood group.
Parents with the first and fourth have a child with the second and third.
Parents with the second and fourth have a child with the second, third and fourth
Parents with third and fourth- a child with the second, third and fourth.
Parents with the fourth have a child with the second, third and fourth.
If one of the parents has the first blood group, the child cannot have the fourth. And vice versa - if one of the parents has a fourth, the child cannot have a first.
Antigen B matures by the age of one year, so it is sometimes not detected at birth. As a result, a child with the third blood group may receive the first blood group at birth, while a child with the fourth may receive the second. By the age of one year, the antigen matures and the blood type “changes.”
Group incompatibility:
During pregnancy, not only Rh conflict (cm) can occur, but also blood group conflict. If the mother has the first blood group, and the child has any other, she can produce antibodies against it: antiA, antiB. It is necessary to check the presence of group antibodies in women with the first blood group, and in the presence of immune antibodies, warn pediatricians about the possible development of hemolytic disease of the newborn based on blood group.
Rh factor
Protein on the membrane of red blood cells. Present in 85% of Rh-positive people. The remaining 15% are Rh negative.
Inheritance: R - Rh factor gene. r - absence of Rh factor.
Parents are Rh positive (RR, Rr) - the child can be Rh positive (RR, Rr) or Rh negative (rr).
One parent is Rh positive (RR, Rr), the other is Rh negative (rr) - the child can be Rh positive (Rr) or Rh negative (rr).
The parents are Rh negative, the child can only be Rh negative.
The Rh factor, like the blood group, must be taken into account when receiving blood transfusions. When the Rh factor enters the blood of a Rh-negative person, anti-Rh antibodies are formed to it, which glue Rh-positive red blood cells into coin columns.
Rhesus conflict
It can occur during the pregnancy of an Rh-negative woman with a Rh-positive fetus (Rh factor from the father). When fetal red blood cells enter the mother's bloodstream, anti-Rh antibodies are formed against the Rh factor. Normally, the blood flow of the mother and fetus mixes only during childbirth, so a Rhesus conflict is theoretically possible in the second and subsequent pregnancies with an Rh-positive fetus. In practice, in modern conditions, there is often an increase in the permeability of placental vessels, various pathologies of pregnancy, leading to the entry of fetal red blood cells into the mother’s blood during the first pregnancy. Anti-Rh antibodies can also be formed not only during pregnancy, but also through contact with Rh-positive blood. Therefore, anti-Rh antibodies must be determined during any pregnancy in an Rh-negative woman starting from 8 weeks (the time of formation of the Rh factor in the fetus). To prevent their formation, carry out prevention of Rhesus conflict. All Rh-negative women who do not have antibodies to the Rh factor at 28 weeks of pregnancy are given anti-Rhesus immunoglobulin in a dose of 350 mcg in the interval between 28 and 34 weeks of pregnancy. And another dose is given within 72 hours after birth. Immunoglobulin is also administered after any end of pregnancy of more than 8 weeks (miscarriage, abortion, anembryonia, frozen pregnancy, premature birth) and during the amniocentesis procedure. During pregnancy, it is possible to use only imported immunoglobulin preparations, in particular Bay-RoDee. After pregnancy, it is possible to use domestic immunoglobulin, which is better than nothing, but worse than an imported drug standardized in terms of the dose of antibodies.
The Rh factor is an antigen (or protein) that is found on the surface of erythrocytes (red blood cells). It was discovered only about 35 years ago. And at the same time they found out that about 85% of men and women have this Rh factor and, therefore, are Rh positive. And the remaining 15%, accordingly, do not have the Rh factor and are called Rh negative.
IN ordinary life Neither the presence nor absence of the Rh factor plays any special role. It only becomes important in extreme circumstances such as blood transfusion or pregnancy.
- if the expectant mother’s Rh factor is negative, and the father’s is positive, the child can inherit both mother’s and father’s Rh, there is a 50x50 chance;
- if he inherits his mother’s negative, then everything is fine, and there is no danger;
- if mom and dad are negative (this good option), then the child can have both negative and positive Rhesus;
- if father’s is positive and mother’s is negative, then there is a threat of Rh conflict.
Rh conflict is the incompatibility of the blood of the mother and her fetus.
The fetal Rh factor crosses the placental barrier and enters the mother's blood. And her body, “not recognizing the fetus” and perceiving it as something foreign, begins to produce protective antibodies. These antibodies penetrate the placenta and begin to “fight” the red blood cells of the unborn child, destroying them. This can lead to miscarriage if the mother's body rejects the fetus. And to the fact that a large amount of bilirubin will begin to be produced in the blood of the unborn baby, a substance that turns the skin yellow and leads to jaundice in newborns. Bilirubin can also damage the brain of the unborn child and cause problems in the development of hearing and speech. In addition, since the red blood cells in the fetal blood will be constantly destroyed, its liver and spleen will accelerate the production of red blood cells, dramatically increasing in size. In this race, however, they will inevitably lose, and as a result, the unborn child may develop anemia caused by alarmingly low levels of red blood cells and hemoglobin. In addition, Rh conflict can cause congenital hydrops (swelling) of the fetus and even lead to its death.
But, fortunately, science has advanced far, and there are preventive measures and methods of treating Rhesus conflict.
1) You need to find out your blood type and your Rh factor as early as possible, as well as the group and Rh factor of your future father. Sometimes a Rh conflict begins when the blood group of the mother and baby is incompatible, for example, if the mother has blood type 0, and the unborn child has A or B. Fortunately, such incompatibility is less dangerous and does not foreshadow serious complications.
2) If both parents have the same Rh, there is no reason to worry.
3) If mom is negative and dad is positive, she will have to regularly undergo a procedure such as a blood test from a vein. This way, doctors will be able to constantly monitor the amount of antibodies in your blood and notice the onset of Rh conflict. Until the 32nd week of pregnancy, blood should be donated once a month, from the 32nd to
35th - twice a month, and then weekly until the day of birth.
4) If a Rhesus conflict nevertheless begins, then specialists can resort to various measures to save the baby. In some cases, premature birth is caused and an exchange transfusion of blood is done to the newborn - doctors inject him with blood of the same group, but with Rh negative. This operation is performed within 36 hours after the baby is born.
5) It is also possible to reduce the risk of developing Rh conflict during subsequent births. For example, by administering a special vaccine - anti-Rhesus immunoglobulin immediately (within 72 hours) after the first birth or terminated pregnancy. The principle of action of this drug is based on the fact that it “binds” aggressive bodies in the mother’s blood and removes them from her body. After this, they can no longer threaten the health and life of the unborn baby. If for some reason Rh antibodies were not administered prophylactically, such a “vaccination” can be done during pregnancy. The administration of anti-Rhesus immunoglobulin is also done after puncture of the amniotic sac, amniocentesis and surgery for ectopic pregnancy.
Antibodies are developed gradually, so there is a high probability that the first child will be born completely healthy. Antibody concentrations by the end of pregnancy may not reach the level at which fetal damage begins. However, antibodies, once generated, remain in the blood for quite a long time, and therefore the risk of Rh conflict in subsequent pregnancies increases sharply.
In addition, if an Rh negative woman (or even a girl) was once given a transfusion by mistake Rh positive blood, there are already antibodies in her blood, and therefore Rh conflict can develop already during the first pregnancy.
For an Rh-negative woman, there are several rules that can increase the likelihood of a normal pregnancy.
1. Any blood transfusion must take into account the Rh factor.
2. If you have a choice, it is better to get pregnant from an Rh-negative partner.
3. It is necessary to avoid abortions from an Rh-positive man, since antibodies are formed from the very beginning of pregnancy. Therefore, it happens that a woman does not have children, but antibodies are already circulating in the blood, waiting for the appearance of a foreign protein.
4. When pregnancy develops, a Rh-negative woman should register as early as possible and regularly donate blood for Rh antibodies.
5. If a Rh conflict occurs, a woman must carefully follow the obstetrician’s treatment instructions.
To minimize the risk of Rh conflict during a subsequent pregnancy, the interval between childbirth and the subsequent pregnancy should be significant - at least 5-8 years.
From all this we can draw the following conclusion.
If a woman is Rh positive, she cannot have any Rh conflict, because she herself has Rh and antibodies cannot be formed to it.
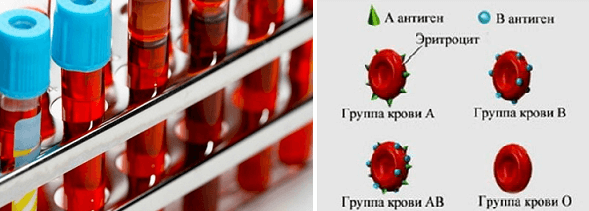
Blood groups are also encoded by special proteins on the surface of blood cells.
Group 1 (0) means the absence of these proteins - “negative” blood.
2 – group A, protein A.
3 – group B.
4 – group AB.
If a woman does not have some protein that her husband has, the child may also have the father’s protein, and a woman who is negative for this protein can form antibodies and act as if they had a Rh conflict. This situation develops much less frequently than Rh conflict, but we also need to remember about it and determine the level of antibodies to blood groups, also starting from 7 weeks of pregnancy.
There may be a conflict if a woman:
1 blood group (0), and in a man – 2 (antibodies to protein A), 3 (to protein B), fourth (to both antitags);
2 (A), and in a man 3 (B) or 4 (AB) - antibodies to antigen B;
group 3 (B), and in men 2 (A) or 4 (AB) - antibodies to antigen A.
So there is no incompatibility in the Rh factor and blood groups as such, and different Rhesus factors do not mean the inability to get pregnant and bear a healthy child.
At the beginning of the last century, people learned that the biological fluid flowing through their veins is not the same. The donor was an ordinary person from whom plasma was taken and transfused to someone who needed it.
But cases of death were not uncommon, since the donor’s plasma may not match that of the recipient (recipient). As it turned out, there are varieties of human blood groups, and there is also such a thing as the Rh factor, and the fact that it can be negative or positive.
Now in our century, parents have increasingly begun to think about what blood type their child will have. The fear of the so-called Rhesus conflict is especially great among pregnant women. This article will help dispel many doubts about heredity.
To understand everything, you need to remember genetics from the school curriculum. This is not a biology course; you are not forced to go back and delve into genetic connections in rabbits and peas. We will try to tell everything simply and easily for your understanding.
Scientists have discovered that when mixing several samples, during transfusion (relevant in hospitals or if you are a donor), knowing which type belongs to a certain type is of no small importance.
How many blood types are there? How do you know how they differ?

There are only four of them. According to the ABO system, they are divided according to the presence of antigen markers A and B. The first does not have them at all, so it is designated as (O). The second and third types contain only one antigen, but the fourth type contains both antigens.
- 1 blood group (IO)
- 2 blood group (IIA)
- 3 blood group (IIIB)
- Blood group 4 (IVAB)
During life, type membership cannot change. The frequency of blood groups may vary. It is believed that best group– the first blood group, or rather, it is the most common, since it is older than the others. Then the second and third, then the fourth.
But this does not give reason to believe that others are worse. Calculating their popularity is a fool's errand. We cannot judge a person by the red liquid flowing through his arteries. Many people attach great importance to this, although in life it is just a trifle, a “serial number.”
The genetics of blood groups is a complex system. Mendel's genetic law describes the principles of inheritance of certain characteristics of a child's blood type, depending on the blood type of the father and mother.
This law helps to understand the principle of how genes can be transmitted and whether blood group compatibility is important for conception. Often the inability to conceive and miscarriages, especially in early stages, do not always indicate physiological problems of partners. Let's figure out what's the matter.
To establish how the blood type and Rh of a newborn are transmitted, you can look at the table. A blood group chart helps you calculate how children will inherit the factors and blood types of their parents. But only laboratory analysis can help determine it 100%.
Below are options with a probability of no more than 75%. Because genes and their mixing cannot be predicted accurately. But such a probability contributes to understanding the whole essence of this “problem”.
Child group inheritance table
| I | II | III | IV | |
| I | I | I, II | I, III | II, III |
| II | I, II | I, II | I, II, III, IV | II, III, IV |
| III | I, III | I, II, III, IV | I, III | II, III, IV |
| IV | II, III | II, III, IV | II, III, IV | II, III, IV |
Inheritance of blood groups is a complex biological process that will be difficult for a person without a higher biological education to understand. But based on this table, we can conclude: if the mother’s blood type is second and the father is also a carrier of the second, then the child can inherit both the first (25%) and the second (75%).
Therefore, you should not be surprised if the child’s name is not yours. If you (IO) and the other spouse have a rare blood type (IV AB), then the second or third blood group may be passed on to your child. This is interesting, since the parents did not have a 2nd or 3rd one, and the child will receive one of them.
In addition to the ABO blood group system, there is the Rhesus (Rh-Hr) system.
What is Rh factor
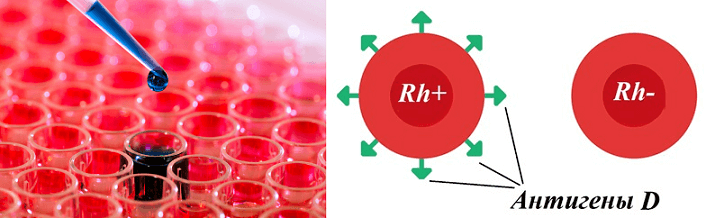
Rh factor (Rh) is a D-antigen, knowledge of the presence of which on red blood cells is necessary during transfusion. This system was discovered back in the 1940s by Landsteiner and Wiener, conducting experiments on macaques (rhesus monkeys). If a person does not have antigens (protein in red blood cells), then he is (-), and if they are present, then (+). He cannot change himself, but he can influence various moments, especially during transfusions and pregnancy.
If Rh(-) is negative, she should alert doctors and get tested for antibodies. If the fetus has a different Rh (for example, “+”), then it is possible to develop antibodies that can lead to Rh conflict.
This especially happens when Rh negative mother. To prevent a conflict from occurring, doctors inject agglutinating antibodies, which reduce the risk of the body producing its own antibodies that interfere with the fetus.
Knowing this, doctors will take the necessary measures during childbirth and be more attentive to you and your newborn. And also, a donor (donor plasma) and the necessary medications will be ready. It’s easier if the mother has Rh (+). Then, if a child’s blood type is Rh (-), there is usually nothing to worry about, because even the antibodies developed, as a result of the difference in Rhesus, will not cause problems, because the mother has them.
Rh factor inheritance table
| Father's Rh factor | |||
| Rh(+) | Rh(-) | ||
| Rh factor mothers |
Rh(+) | Rh(+) | Rh(+) |
| Rh(-) | Rh(-) | ||
| Rh(-) | Rh(+) | Rh(-) | |
| Rh(-) | |||
More than 85% of people (Caucasians) – positive group blood, that is, they have D-antigens on their red blood cells. If the donor is “-” (negative Rh), then he can give a positive “+” transfusion. But in no case is it the other way around. Because “negatives” do not have antigens, and this fact can have terrifying consequences, even death.
As we already understood, the Rh factor influences the determination of compatibility during transfusion and pregnancy. The donor must also donate the Rh factor. The fourth negative is the rarest, but do not be afraid, in the event of a transfusion, doctors will find the right amount and the right donor. Also, during transfusion, samples from the donor and recipient are mixed, thereby checking compatibility.
D-antigens can be mixed and inherited by a child in almost any combination. Many, not knowing the laws of genetics and how blood type is inherited, needlessly accuse their wives or daughters-in-law of infidelity. Although in fact, husbands and mothers-in-law are wrong, due to their lack of education and lack of awareness of science.
Where can I find out my blood type? Scientists have not yet come up with signs by which this could be determined independently at home. But it is possible to do this in any laboratory where they will test your blood group and determine your Rh status. The procedure has changed many years later; now it is simple and does not take much time.
In general, it is good to know what your blood type and Rh factor are. In the future, it will be possible to reduce the time for additional tests. At birth, this analysis is mandatory, and local clinics issue a medical card that contains all this data, which cannot be changed.



