The vast majority of people who are far from medicine know very vaguely that there is a Rh factor, since the quality everyday life it doesn't have any effect.
However, everything changes during the period when a woman is carrying a child: negative Rh during pregnancy can become the main cause of the onset of Rh conflict. This phenomenon occurs quite rarely (statistically, less than 1% of pregnant women experience this), but this does not make the problem less serious and significant: in some cases, the conflict can even lead to the death of the child.
But the development of modern medicine makes it possible to give birth normally and not with such problems: the main thing is to seek qualified help from a gynecologist, who will tell you what to do.
Rh factor is a type of protein that is located on the surface of red blood cells. If present in a person, it is called Rh positive. If it is absent, it is Rh negative.
When an Rh-negative woman decides to become pregnant with a Rh-positive man, the child's Rh factor may become Rh positive. As a result, a Rh conflict can occur with serious complications for the fetus or newborn child, including death.
When a woman registers for pregnancy, the gynecologist must give a referral for a blood test to clarify the Rh factor of the mother and fetus. This is done in order to identify the threat of Rh conflict in time and begin to prevent it.
Causes of Rh conflict
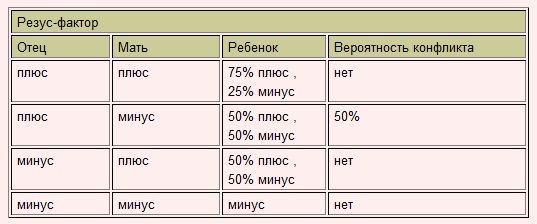
A “positive” mother does not have an Rh conflict with the fetus under any circumstances, and the father’s Rh is in in this case doesn't matter. But if the pregnant woman’s blood turns out to be Rh negative, the blood type and Rh affiliation of her husband are determined. If the unborn baby's mother and father are Rh negative, there is nothing to worry about. The baby will also be born Rh negative. There simply cannot be any conflicts in this case! But if the parents are Rh positive, the child in the vast majority of cases will have Rh protein in the blood (as already mentioned, it is transmitted as a stronger trait).
Rh conflict can occur during pregnancy if the mother's Rh factor does not match the fetus' Rh factor.
In the case where the carrier positive Rh factor the baby is born, the likelihood of a Rh conflict occurring is much higher, and its consequences are much more serious.
In addition to the Rh factor, a conflict may develop if the blood of the expectant mother and child are incompatible in blood type.
What is the essence of Rh conflict? Watch the video:
Group incompatibility develops if the mother has the first blood group - 0 (I), and the child has the second A (II) or the third B (III).
In most cases, a woman's first pregnancy Rh negative blood- Rhesus fruit positive blood goes normally, however, even with a repeat similar pregnancy, the likelihood of Rh conflict increases sharply. At the same time, it is of considerable importance how your previous pregnancy ended, which arose with the risk of Rh conflict.
Antibody formation usually occurs: 
- in 3-4% of cases after a miscarriage
- in 5-6% after abortion
- in 1% of cases after ectopic pregnancy
- in 10-15% after normal birth
Also, the risk of antibody formation increases if you have had or been observed to have a condition that caused placental abruption. From all this it follows that the risk depends on how many fetal red blood cells enter the mother’s blood.
Donating blood for antibodies
For the sake of the safety of her baby, an expectant mother with negative Rh blood must come to terms with the fact that she will have to take a blood test for antibodies often.
Until 32 weeks of pregnancy, this must be done weekly, from 32 to 35 - once every two weeks, and from 35 to 40 weeks - again weekly. Such monitoring will show the doctor leading the pregnancy how the composition of the blood changes.
If the number of antibodies begins to increase, this means that the baby’s life is in danger and urgent measures must be taken.
You can learn more about what risks there may be for mother and child with negative Rhesus in the video:
Signs of Rh conflict
Rh incompatibility with fetal blood does not affect the health of the mother. Complications appear only in a newborn baby. Fetal pathology can be diagnosed using, during which the following signs are detected:
- accumulated fluid inside the fetus;
- swelling and enlargement of the placenta;
- increased size of the child's abdomen;
- swelling;
- flexion of the fetal legs in a characteristic position;
- discrepancy in the size of internal organs;
- swelling of the head.
Risks for the child
 Rh conflict can lead to complications for the fetus. First of all, this is anemia, swelling of internal organs and tissues, in particular the brain. In complex cases, erythroblastosis and hepatitis may develop.
Rh conflict can lead to complications for the fetus. First of all, this is anemia, swelling of internal organs and tissues, in particular the brain. In complex cases, erythroblastosis and hepatitis may develop.
The child may develop dangerous hemolytic disease. Particularly difficult cases include the development of dropsy and edema syndrome, which can lead to missed abortion or stillbirth. To avoid such consequences, to the expectant mother it is necessary to be constantly monitored by a doctor.
How to give birth with a negative Rh factor
Prepare for conception in advance. Take a blood test to determine antibodies to determine whether the system has been immunized with Rh (+) blood. It is appropriate to do such an analysis before the 28th week of pregnancy.
If the baby's father has Rh (+), a pregnant woman who is Rh-negative is given an injection of anti-Rh immunoglobulin on the 28th.
This injection will have to be repeated at 7 months if the pregnant woman experienced bleeding during pregnancy or amniocentesis was performed. Also, the drug is administered again after childbirth for 2-3 days. If the mother and father have (-) blood, these procedures will not be necessary.
The doctor is obliged to carefully monitor the course of pregnancy with complications. He decides whether the pregnant woman will be able to carry the child to term and give birth on time, or whether labor will have to be induced ahead of schedule.
Most effective way treatment - an intrauterine blood transfusion procedure performed in a hospital. This procedure significantly reduces the likelihood of pathologies and early birth.
Additionally, doctors fear premature placental abruption and other problems. Tactics are determined individually, taking into account the severity of the Rh conflict, but usually pursue the following goals: 
- avoid damage to maternal tissue as much as possible;
- exclude labor stimulation, which increases the risk of fetal blood entering the woman’s bloodstream;
- it is possible to prescribe an early amniotomy (intra-amniotic pressure decreases);
- According to indications, it is mandatory to prescribe medications;
- delivery can be carried out through the natural birth canal if there are no contraindications.
- prescribing a caesarean section according to indications;
- delivery can take place as early as 37-38 weeks due to a greater supply of Rh antibodies to the fetus towards the end of pregnancy;
- if hemolytic disease is detected, then delivery is possible at an earlier date;
- the umbilical cord is crossed immediately;
- blood is immediately taken from the baby to determine the content of bilirubin, hemoglobin, blood type and Rh factor;
- the umbilical cord remains are formed in the correct way.
First, a little background on this post: I have a friend Lena - a walking “complete medical encyclopedia,” but that’s not what I’m talking about now. During her first pregnancy, it turned out that she had blood type II, and the Rh factor was negative (while her husband was positive). So Lena became a “rhesus-conflicted” pregnant woman. (Rh conflict is an immune reaction in which the mother’s body produces antibodies directed against the child she is carrying).
The pregnancy was difficult, the young mother practically did not leave the hospital and heard a lot: about retinal detachment, and about congenital dropsy, and about the fact that either she or the baby would be saved during childbirth...
But everything went more or less smoothly: Yulka was born - a smart, smart girl. Everything seemed to be fine. But things didn’t work out with her husband, and Lenka was left alone with her daughter. Young and beautiful, she then told me that if she ever gets married again, then before that she will look in the passport of her chosen one so that there is a note about the negative Rh factor.
Soon what was predicted came true: Lena got married again, having previously kept her promise - her new husband had I negative group blood.
Then they had a son. The pregnancy proceeded calmly, the doctors did not bother Lena, since both parents have a negative Rh factor.
Imagine Lenkina’s surprise when, the day after giving birth, she was informed that the baby had I positive group! The doctor insisted that even theoretically this could not happen with both “negative” parents, and advised her husband not to tell him, which greatly hurt Lenka’s pride. She began to insist on repeat tests because she was sure of paternity.
And then two days later she was told another piece of news - her husband’s blood was positive! "Defective!" - that was all Lenka, exhausted from her experiences, could say to her dumbfounded husband as she left the maternity hospital.
How could this happen? Whether the stamp was confused with the blood type in Lenin’s husband’s passport, or whether, as some people claim, the blood type is actually capable of changing with age, it is not clear. The fact is that Lena was again “Rh-conflicted” throughout her pregnancy, but no one even took control of her! Moreover, this was the second pregnancy (it is believed that in the likelihood of problems with each subsequent pregnancy increases, since protective antibodies from the previous child remain alive in the mother’s body).
This example once again proves that the lies about the fact that boys die due to Rh-conflict, that it is impossible for a mother to bear a healthy baby with negative Rh factor impossible.
It seems strange to me that women often find out their blood type when they are already pregnant during their first visit to the antenatal clinic. After all Approximately 15% are Rh negative of them, i.e. every seventh! And they need to plan their pregnancy!
If the likelihood of conflict during the first pregnancy is about 10%, then with each subsequent one it increases by another 10%. The same can be said about any interventions when Rh-positive blood cells enter the blood of an Rh-negative mother: artificial or spontaneous abortion or ectopic pregnancy, transfusion of Rh-incompatible blood even in early childhood, bleeding during pregnancy, manual separation of the placenta, cesarean section. section, significant blood loss.
Therefore, Rh-negative women need to be especially attentive to their health: make sure that there was no “meeting” with Rh positive blood
(in particular during an abortion or miscarriage), in such cases it is necessary to urgently administer a drug that inhibits the production of antibodies. It is believed that carrying the first pregnancy is optimal.
During pregnancy, you will have to donate blood quite often to determine the level of antibodies. You may need to administer anti-Rhesus immunoglobulin, which prevents the mother from forming antibodies that reject her own child, or hospitalization in a perinatal center.
But remember Lenka - Rh incompatibility is not at all an obstacle either to love or to the birth of children. With the right approach, the risk can be reduced not only to a minimum, but to none!
And one more thing - Rh conflict arises only when OThe father is Rh positive and the mother is Rh negative(and only if the baby inherits the dad’s Rh factor). And in no other case!
What is the danger of negative Rh blood in a woman during pregnancy? What precautions should you take? What do experts advise? Littleone collected useful information about Rh conflict between mother and child.
What is the cause of the conflict?
Rh negative in itself does not affect a person’s health or quality of life. It becomes a risk factor in one and only case: when a woman becomes pregnant. If the mother has negative Rh blood and the father has positive Rh, the child may inherit his Rh. In this case, a Rhesus conflict will arise between mother and child. The cause of the conflict is a protein found in red blood cells (Rh factor). Approximately 85% of people have it (Rh factor is positive), and the remaining 15% do not have it (respectively negative).
What's happening?
If fetal red blood cells with an antigen protein enter the blood of a mother with a negative Rh factor, the body perceives them as foreign and begins to produce antibodies to destroy the child’s red blood cells. A child develops a high amount of bilirubin in his blood, which can damage his brain function. To replenish the number of constantly destroyed red blood cells, the child’s liver and spleen begin to work actively, while increasing in size. But they do not always cope, and a failure in their work can lead to new serious disorders, including oxygen starvation, congenital dropsy and fetal death.

So, you can’t get pregnant if your parents have different Rh factors?
As a rule, the first pregnancy for an Rh-negative mother and Rh-positive father goes smoothly, although under close medical supervision. If a woman’s body has not previously encountered “enemy” red blood cells, then she does not have antibodies that could lead to an Rh conflict with the child, or their number is not significant. However, at the same time, “memory cells” remain in the woman’s blood, which in subsequent pregnancies are able to quickly begin to produce antibodies against the Rh factor.
What can be done?
First of all, be careful. When registering, a pregnant woman is checked for the Rh factor. If it is negative, they will find out the Rhesus status of the child's father. In case of a possible Rh conflict (the father is Rh positive), doctors monitor the amount of antibodies in the woman’s blood. Until the 32nd week, a blood test for antibodies is taken once a month. From the 32nd to the 35th week inclusive - twice a month, then weekly until the birth.
In many ways, the degree of risk of Rh sensitization (antibody production) depends on how the first pregnancy ended. After a miscarriage or ectopic pregnancy, the risk is relatively low - 1-4%. In the case of a successful delivery, the figure is higher - 15%. At caesarean section or placental abruption, it increases. Simply put, the more red blood cells from a child enter the mother’s blood, the higher the risk.
Immediately after birth, doctors determine the baby's Rh factor, and if it is positive, the mother is given anti-Rhesus immunoglobulin, preventing the development of Rh conflict in subsequent pregnancies.
Important! Anti-Rhesus serum should be available in all maternity hospitals, regardless of whether they specialize in Rh-conflicts or not. But in practice this rule is not always followed. It will be better if you find out in advance whether the maternity hospital you choose is equipped with this serum. If it is unavailable, doctors recommend purchasing serum in advance.
Also, prophylaxis with anti-Rh serum is carried out within 48 hours after an ectopic pregnancy, spontaneous or artificial termination of pregnancy, trauma to a pregnant woman or transfusion of Rh-positive blood.

What additional procedures may be prescribed?
- Blood test
When registering, an Rh-negative woman will be prescribed an additional blood test for antibodies, their quantity, and antibody titer. If no antibodies are detected, the next titer blood test will be scheduled at 18-20 weeks of pregnancy. In the absence of antibodies, at the 28th week the expectant mother will be given anti-Rhesus serum.
If antibodies are detected, the pregnant woman will be tested for their quantity regularly: monthly until the 32nd week, once every two weeks from the 32nd to 35th weeks, weekly from the 35th week until delivery.
- Doppler
Assigned, as a rule, in the third semester. During the examination, the specialist will check the pressure in the vessels to determine the risk of blood stagnation and thrombosis. The procedure shows the level of blood flow in the vessels of the placenta and umbilical cord and in the uterine arteries. A decrease in blood flow, on which the child’s oxygen supply, growth and development depends, may be a sign of a deterioration in the baby’s condition.
- Ultrasound examination (ultrasound)
The study allows you to notice in time the first signs of the beginning attack of maternal antibodies: thickening of the placenta, an increase in the amount of amniotic fluid, a sharp increase in the size of the child’s liver and spleen.
- Cardiotocography (CTG)
A hardware test that monitors and records on a special tape the fetal heart rate. The child’s heart tone, if it increases or slows down, can become a symptom of a deterioration in the baby’s well-being.
- Intrauterine intervention (cordocentesis, amniocentesis)
It is carried out when the number of antibodies sharply increases and the child’s well-being deteriorates. Under ultrasound control, 20 to 50 ml of group I donor Rh-negative blood is injected into the child’s umbilical cord or fetal bladder cavity through the anterior abdominal wall of the mother. This will lead to a weakening of the woman’s immune response and a decrease in the number of Rh-positive red blood cells, due to which the child’s condition will improve.
Cordocentesis can be performed several times until the 34th week. After this period, the child is considered viable, and the question of early birth may be raised.
- Skin grafting
In the last trimester of pregnancy, the mother can have a piece of the future dad's skin implanted. This is a kind of distracting maneuver: when a piece of tissue takes root, the woman’s body will perceive it as foreign and will throw all its strength into the fight, while being distracted from the production of antibodies to the child’s Rhesus, which will give doctors the opportunity to prolong the pregnancy.
- Anti-Rhesus serum
We wrote about it above: when positive rhesus In the first 48 hours after birth, doctors administer immunoglobulin to the mother. The serum reduces the likelihood of Rh conflict in subsequent pregnancies.

Personal experience of forum members
- with severe Rh conflict.



